How Plaques in Arteries Form, Grow and Rupture
The silent decades-long process that leads to heart disease and stroke.
When a heart attack happens, many victims experience radiating pain from their chest to their arms and other parts of the body. You may also experience a squeezing feeling across your chest, dizziness, and shortness of breath among other symptoms.
While a heart attack may feel like a sudden health condition that has come out of the blue, these symptoms are actually the culmination of a decades-long silent process called atherosclerosis or plaque formation.
In this post, we look at how fats and cholesterol buildup in arteries in a process called atherosclerosis. We also discuss how it leads to health problems like stroke, heart attack and heart failure.
Hi 👋, Isaac here. I publish Man Science. Leave a tip at Buy Me a Coffee to help keep this newsletter free for everyone. And if you are not yet a subscriber, tap the button below
What is Atherosclerosis?
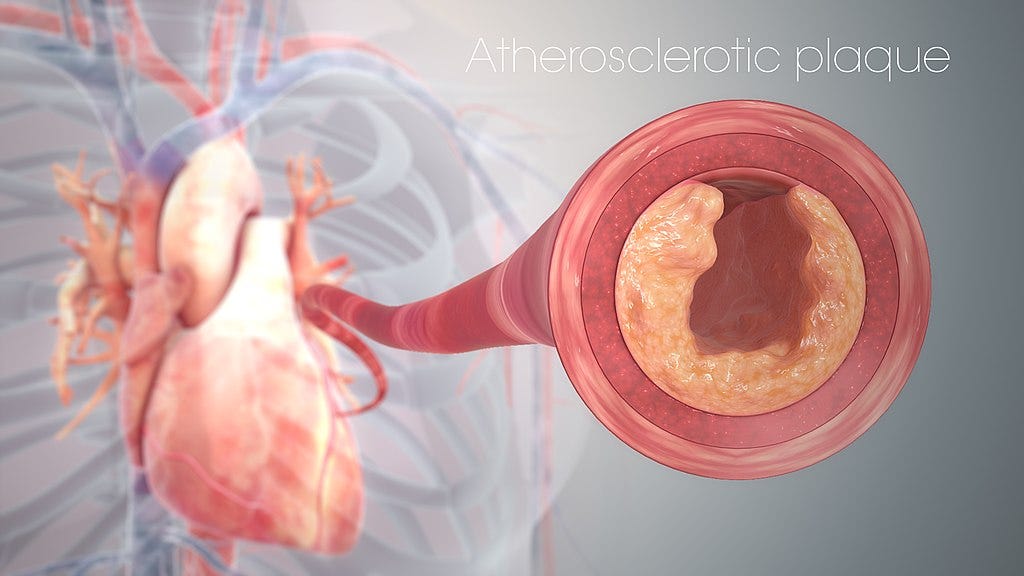
The process of plaque formation and growth is called atherosclerosis. These plaques consist mostly of accumulated fats, most of which is low density lipoprotein (LDL), or what we normally call bad cholesterol.
Plaques also contain immune cells, which drive inflammation and cause the plaques to grow larger.
Other components of plaques include collagen (a type of protein fiber), dead or dying cells, and calcium deposits.
As plaques grow larger, arteries become narrower and stiffer. This makes it harder for blood to flow through leading to chest pain (stable angina), high blood pressure (hypertension), peripheral artery disease and other problems associated with poor blood flow.
The heart also has to work harder to pump blood. This can cause the heart muscles to thicken and stiffen, increasing the risk of irregular heartbeat and heart failure.
Xanthomas: The First Stage of Plaque Formation
Researchers are not fully sure what causes plaques to start forming in the arteries. The most accepted explanation is the response-to-injury hypothesis.
This hypothesis says that atherosclerosis begins with an injury to the inner wall of an artery. The arteries most at risk include coronary arteries (supplying blood to heart muscles), abdominal aorta, iliofemoral arteries (supplying blood to the legs and feet) and carotid arteries (supplying blood to the brain).
The initial injury can be caused by various things including:
Smoking
High blood pressure
An infection such as chlamydia
Type 2 diabetes
As with any other injury in the body, there is an inflammatory response. Immune cells called monocytes flood the area to repair the damage. This is a normal immune response.
When monocytes get to the injury area they turn into macrophages, which are mature versions of monocytes. Again, this is still a normal process. Next is where things start to haywire.
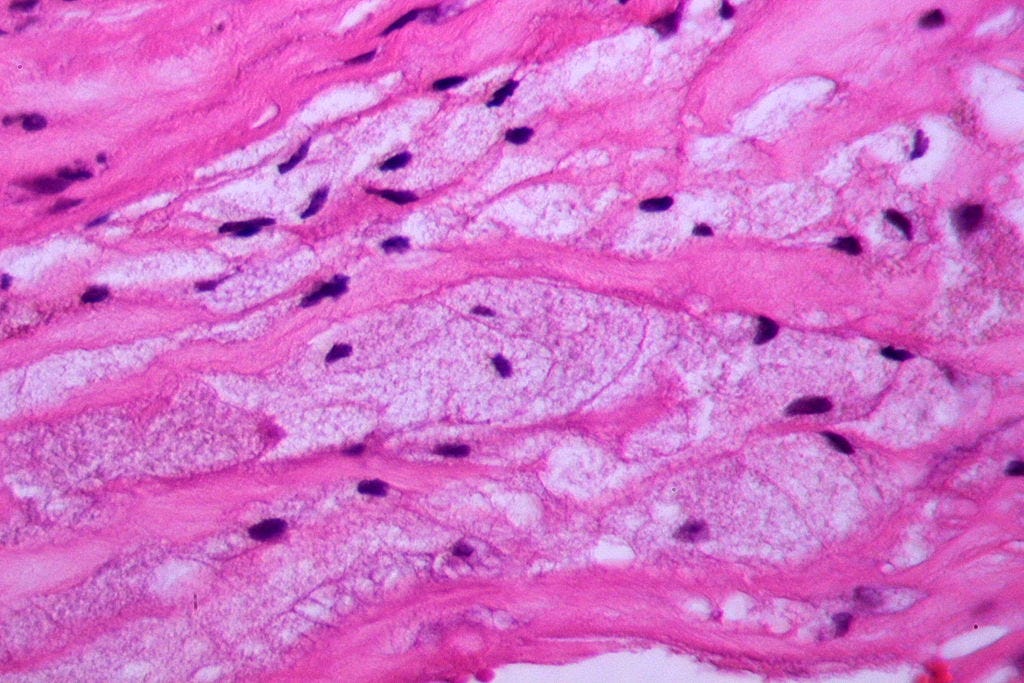
These macrophages engulf and ingest or ‘eat’ droplets of LDL cholesterol that are in the blood and trapped in the walls of the artery. As the macrophages fill up with lipids, they turn into foam cells. They literally appear foamy, hence the name.
Researchers have found that plaques are more likely to form on parts of the artery that have a thicker wall. Normally, parts of arteries will thicken in response to stress and pressure from blood flow. This is called adaptive intimal thickening.
Areas with adaptive intimal thickening have more smooth muscle cells than other areas of the artery. Smooth muscle cells (SMCs) control the contraction and dilation of blood vessels to regulate blood pressure and flow.
SMCs produce substances called proteoglycans that provide structural support to tissues and organs. It is likely that proteoglycans play a role in trapping cholesterol, thus making it easier for macrophages to ingest them.
That may explain why plaques are more common in areas with adaptive intimal thickening — they have more smooth muscle cells, and thus more proteoglycans.
When foam cells begin to accumulate, they form lesions (areas with an abnormal appearance) called xanthomas. This is the first stage of atherosclerosis.
Xanthomas are harmless and reversible. In fact, they can appear as early as infanthood or even in fetuses, likely caused by the health of the mother.
But they go away on their own, often reappearing in adolescence.
How Plaques Grow and Turn Deadly
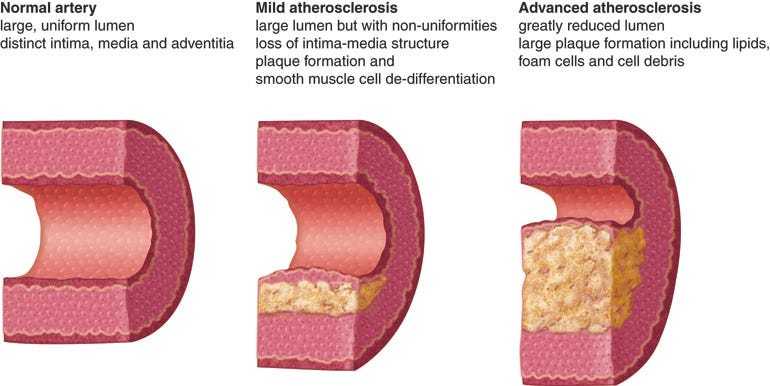
As foam cells increase, pools of cholesterol (mostly LDL or bad cholesterol) start forming under them. These are called lipid pools and they cause the walls of the artery in the affected areas to grow even thicker.
This is called pathological intimal thickening. Pathological means it’s caused by a disease unlike adaptive intimal thickening which is a natural and normal response.
Pathological intimal thickening sets in between the ages of 20 and 30. At this point, these changes don’t yet have a major effect on the structure or function of the arteries.
The next step is where things get irreparably worse.
Macrophages invade the lipid pool, forming more foam cells. These foam cells along with smooth muscle cells then undergo cell death (through necrosis and apoptosis - both are types of cell death).
At the same time, the body’s mechanism for clearing away toxic dead cells, called efferocytosis, doesn’t function properly in the areas where plaques are forming. That’s likely because the neighboring phagocytes (immune cells responsible for efferocytosis) also die and get dumped in the lipid pool.
So you have lipids and dead cells accumulating inside a plaque. They eventually form what’s called a necrotic core.
When there is a necrotic core, that’s officially a plaque. It’s also called a fibroatheroma.
The space between a necrotic core and the surface of a plaque consists of fibrous tissue, most of which is collagen. There are also proteoglycans and elastin. All these are types of structural proteins produced by smooth muscle cells.
The Necrotic Core
The development of a necrotic core is the main precursor to heart disease. That’s because it causes further growth of plaques and increases the risk of deadly consequences should the plaque rupture.
A necrotic core causes even more inflammation by attracting additional immune cells to the plaque. These cells enter through new and delicate blood vessels that feed into the plaque. These vessels often burst, causing further inflammation and adding to the cellular debris in the necrotic core. This is called intraplaque hemorrhage and it’s a major factor in the growth and instability of plaques.
As it grows bigger, the necrotic core makes the plaque more likely to burst and cause clots that block the artery. It does this by causing instability (e.g. through intraplaque hemorrhage) and by eating away at the fibrous cap/covering of the plaque. A thin fibrous cape greatly increases the risk of plaque rupture.
The presence of a necrotic core makes it more likely for deadly clots to form when the plaque bursts. That’s because the necrotic core is highly thrombogenic, meaning it easily causes blood to clot.
A necrotic core can also lead to calcification. It traps calcium deposits. These can grow larger over time and contribute to heart disease.
Plaque Rupture and Thrombosis
Plaques can eventually get big enough to obstruct blood flow to the heart and other areas of the body. But this rarely causes death. Usually, the only symptom is chest pain or stable angina. You feel pain or pressure on your chest when you are stressed or physically exert yourself. It goes away with rest.
Most plaques remain stable and asymptomatic.
A few plaques, however, have a thin cap. These are called thin cap fibroatheromas or TCFAs. A tear or gap can easily form on the cap, either spontaneously or triggered by stress, physical exertion (e.g. exercise or sex), or a traumatic event such as an earthquake.
This gap exposes blood to the lipids and dead cells inside the necrotic core, causing clotting, also called thrombosis.
Most plaque ruptures are not deadly and can even happen without any symptoms. The clots are small and are quickly broken down by the body.
Factors that determine how dangerous a plaque rupture is include:
How thrombogenic (likely to cause clotting) the plaque material is.
How much the clot disrupts blood flow. The more blockage a clot causes, the more dangerous it is. Partial blockage may only cause chest pain while full blockage results in a heart attack or stroke.
Systemic thrombogenic propensity - how likely clotting will occur anywhere in your body. Smoking and existing health problems such as diabetes and high blood pressure increase thrombogenic propensity, meaning they can make it more likely for large clots to form when a plaque ruptures.
Heart Diseases
When a plaque ruptures and clots form, it leads to different types of heart diseases.
The most common is acute coronary syndrome that occurs when a clot obstructs blood flow to the heart muscles. Without enough blood, and the oxygen and nutrients it brings, heart muscles cannot function properly.
This can cause myocardial infarction, or what we commonly call a heart attack.
It can also lead to unstable angina. This is a type of unpredictable chest pain (occurs even when at rest) that’s usually a warning sign of an impending heart attack.
Plaque ruptures and heart attacks can also lead to sudden cardiac arrest, which can cause death in minutes.
Sudden cardiac arrest or heart failure is different from a heart attack. A heart attack happens when a clot obstructs blood flow to the heart. Sudden cardiac arrest is the sudden malfunction of the heart, causing it to stop beating. The heart’s electrical system that regulates pumping stops working.
A heart attack increases the risk of cardiac arrest happening in the future. A clot from a plaque rupture can also cause irregular heartbeat (arrhythmia) leading to sudden cardiac arrest.
Plaque formation in arteries can also make heart muscles grow thicker, a condition called ventricular hypertrophy. That’s because the heart has to work harder to pump blood.
As the muscles grow thicker and stiffer, the risk of sudden cardiac arrest goes up.
Plaque rupture can also interrupt blood flow to the brain if it occurs in the carotid artery. This leads to stroke.
Heart Diseases are Preventable
While there are ways to treat heart diseases including surgery, stents and medications, the best option is prevention.
Heart disease is preventable through a heart-healthy lifestyle. Stay active, eat a healthy diet, avoid smoking, reduce stress levels and watch out for risk factors like diabetes and hypertension.
The reason heart disease kills so many people is that it progresses silently. Without symptoms, people don’t take preventive measures until it is too late.
So even if you feel healthy, maintain a healthy lifestyle.
P.S. Deaths from heart disease have gone down, though it is still one of the leading causes of death. One reason for this is reduction and better management of risk factors like smoking, diabetes and hypertension. It’s also because more people are surviving heart attacks. But as populations in many developed countries age, the prevalence of heart disease will likely increase.
P.S. (2) In the article, I have only talked about plaque rupture as the main mechanism behind clot formation and heart disease. There’s another process called plaque erosion that contributes significantly to heart disease. Researchers don’t fully understand how it happens, but it involves the gradual wearing away of the fibrous cap covering a plaque.



